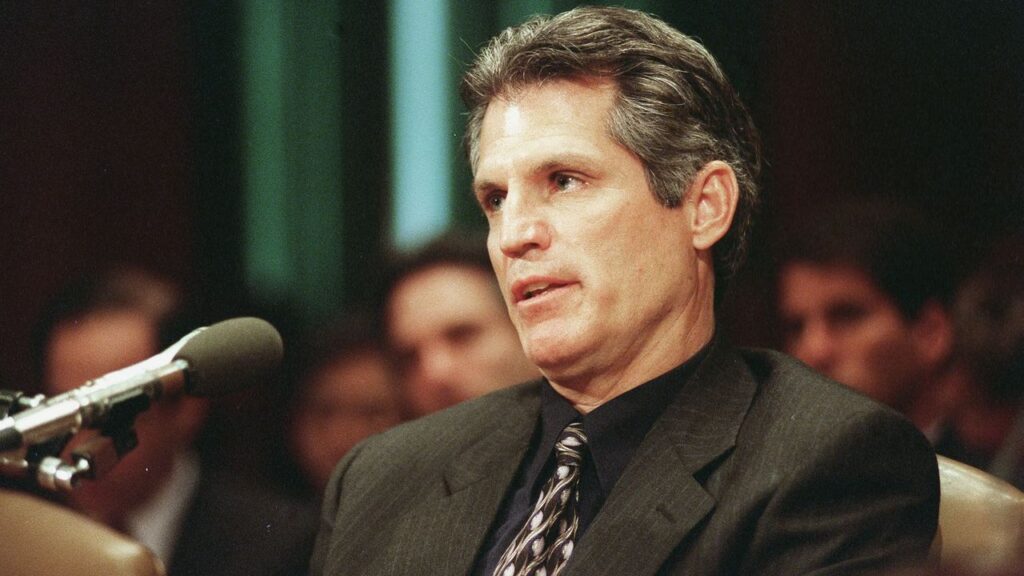
UNITED STATES - FEBRUARY 02: SENATE PUBLIIC HEALTH SUBCOMMITTEE -- Paul Gelsinger, father of young man killed in gene therapy trial, testifies before the Senate Public Health subcomittee hearing on safety concerns associated with gene therapy. (Photo by Douglas Graham/Congressional Quarterly/Getty Images)
UPDATE: Today marks the 26th anniversary of the tragic death of Jesse Gelsinger, the first reported fatality linked to gene therapy, a turning point that dramatically reshaped clinical trial protocols in the field. On September 17, 1999, the 18-year-old succumbed following an experimental treatment at the University of Pennsylvania, igniting widespread skepticism and halting gene therapy advancements for years.
Gelsinger suffered from ornithine transcarbamylase (OTC) deficiency, a rare genetic disorder that affects approximately 1 in 40,000 newborns, preventing the body from breaking down ammonia—a toxic byproduct of metabolism. Despite managing a milder form of the disease with a strict low-protein diet and medication, Gelsinger enrolled in a clinical trial aiming to correct the faulty gene using a viral vector.
On September 13, 1999, Gelsinger received the infusion intended to deliver the corrected OTC gene. Expected flu-like symptoms quickly escalated into a severe inflammatory response, leading to organ failure. By 2:30 PM on September 17, he was taken off life support. Investigations later revealed that his death stemmed from a severe immune reaction to the adenovirus used in the treatment.
An FDA investigation exposed significant issues with Gelsinger’s trial enrollment, including inadequate liver function and undisclosed prior complications in animal trials. Furthermore, the lead investigator, Dr. James Wilson, had financial stakes in the therapy’s success, raising ethical concerns about the trial’s management.
In the aftermath, Gelsinger’s father, Paul Gelsinger, filed a wrongful death suit, which was eventually settled for an undisclosed amount. The event prompted vital reforms in clinical trial regulations, including enhanced informed consent processes and increased oversight by the FDA, which halted all gene therapy trials at the University of Pennsylvania.
As funding for gene therapy dwindled in the wake of this tragedy, the field stagnated. However, advances in viral vector technology and the emergence of CRISPR gene-editing capabilities revitalized research. Remarkably, in January 2024, the first CRISPR-based therapy for sickle cell anemia gained FDA approval, showcasing the resilience of scientific progress despite past tragedies.
Now, scientists have successfully employed gene therapy to treat numerous rare genetic disorders, including severe combined immune deficiency and various forms of blindness. Most notably, in 2025, researchers announced the first use of customized CRISPR therapy to address a unique genetic mutation in an infant suffering from a severe genetic syndrome.
The field of gene therapy continues to evolve, with a limited number of approved products currently available. Many therapies focus on editing cells in the lab before reintroducing them into patients, rather than directly altering genes in their cells.
The legacy of Gelsinger’s death is a stark reminder of the ethical and safety considerations essential in medical research. While the advancements in gene therapy offer hope for patients worldwide, they also underscore the importance of rigorous oversight to prevent tragedies from recurring.
As the scientific community reflects on this pivotal moment, the progress made in gene therapy serves as a testament to the enduring pursuit of innovation in medicine—a pursuit that ultimately aims to transform and save lives.





