A new blood test called Galleri is making headlines, particularly with its recent commercial airing during this year’s Super Bowl. Priced at $949, Galleri claims to detect hidden cancers before symptoms arise by analyzing cell-free DNA in the blood. The test seeks out specific methylation patterns that indicate the presence of cancer, aiming to provide early warnings for individuals at elevated risk.
Getting tested with Galleri is straightforward. Interested individuals can purchase the test online, visit a testing center for a blood draw, and receive their results in about two weeks. The outcome will either indicate a “cancer signal detected” or “no cancer signal detected.” In practical applications, about 1 in 100 people will receive a positive signal, which suggests a likely tissue of origin, such as the pancreas or colon, helping guide further investigation.
Understanding the Limitations
Despite its promising marketing, experts urge caution regarding Galleri’s effectiveness. The manufacturer, GRAIL, recommends the test primarily for adults aged 50 and older or those with risk factors including smoking, obesity, or a family history of cancer. Nonetheless, the test’s performance and value have not been rigorously studied across all recommended groups, and it is not designed for those currently undergoing cancer treatment.
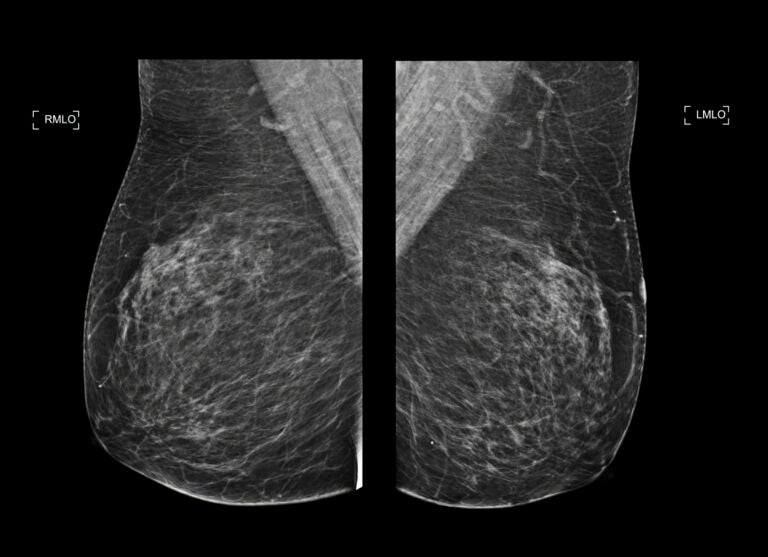
The crux of any cancer test’s utility lies in its performance metrics, particularly its ability to accurately predict the presence of cancer. Unfortunately, Galleri’s sensitivity varies significantly by cancer stage. In studies, it showed a sensitivity of only 16.8% for Stage I cancers, the earliest and most treatable, while sensitivity surged to over 90% for Stage IV cancers, which are typically more advanced and harder to treat.
Another critical issue is the test’s propensity for false positives. Although Galleri boasts a specificity of around 99%, this can still lead to a significant number of false alarms when used in a large, largely healthy population. According to the PATHFINDER study, 62% of positive results were false positives, meaning most individuals with a detected cancer signal did not actually have cancer. This can initiate what medical professionals refer to as a “diagnostic odyssey,” involving extensive and often invasive follow-up procedures, which can introduce considerable stress and financial burden.
The Psychological and Economic Impacts
The consequences of a positive Galleri result can be profound. Patients may undergo numerous tests—such as CT, MRI, or PET scans—over an average span of six months, incurring significant costs and anxiety even when cancer is ultimately ruled out. Conversely, a negative Galleri test can create a false sense of security. In the PATHFINDER study, 71% of cancers diagnosed during the study were identified not through Galleri, but through standard screening methods or via symptoms. This could lead patients to forgo necessary screenings or ignore early warning signs.
While individual cases may illustrate the test’s potential benefits—for example, a 55-year-old receiving a signal indicative of stomach cancer that then leads to successful early treatment—these instances are not the norm. Most cancers detected by Galleri are those for which no standard population-level screenings currently exist, such as stomach, pancreatic, or ovarian cancers. Yet, due to its low sensitivity for early-stage cancers, it remains uncertain whether Galleri can effectively shift diagnoses in a way that improves outcomes on a broader scale.
Currently, no randomized controlled trials have conclusively demonstrated that Galleri testing reduces cancer mortality. History shows that various screening tests can identify diseases without enhancing survival rates, sometimes even causing unnecessary harm through over-diagnosis and over-treatment. Major health organizations have not recommended multi-cancer early detection tests like Galleri for population-wide screening, underscoring the need for further validation through ongoing clinical trials, including the extensive NHS-Galleri study with 150,000 participants.
Moreover, the cost of the test poses a significant barrier. At $949, Galleri may only be accessible to those with disposable income, exacerbating existing disparities in healthcare access. Many proven screening methods remain underutilized in underserved communities, highlighting a troubling divide in the availability of necessary health services.
While some patients may choose to pursue Galleri testing, motivated by a desire for comprehensive health knowledge, it is essential that they engage in thorough discussions with their healthcare providers beforehand. Such conversations should encompass the statistical realities, including the risks of both false negatives and false positives, as well as a clear plan for the potential diagnostic journey that may follow a positive result.
As research continues to evolve, the vision of intercepting various cancers through a simple blood draw remains an enticing prospect. However, the current evidence suggests that Galleri and similar tests fall short of delivering the promised benefits. Ultimately, the most effective strategies for reducing cancer risk often revolve around lifestyle adjustments, such as adhering to guideline-recommended screenings, quitting smoking, maintaining a healthy weight, moderating alcohol intake, and promptly addressing persistent symptoms.