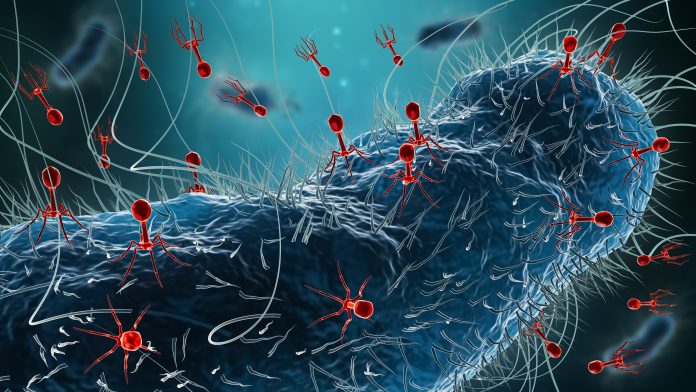
Research has uncovered a substantial number of previously unidentified phages within the human gut, potentially reshaping our understanding of gut health and its implications for various diseases. A study published in the journal Nature titled “Isolation, engineering and ecology of temperate phages from the human gut” represents a pioneering effort in this area, using a comprehensive culture-based approach to isolate and study temperate bacteriophages.
Jeremy Barr, PhD, a professor at Monash University’s School of Biological Sciences, emphasized the significance of the research. “This is a foundational study that changes how we think about and study the viruses within the human gut,” he stated. The team discovered that compounds produced by human gut cells could activate dormant viruses residing within gut bacteria. This finding could have important implications for conditions like inflammatory bowel disease (IBD), where inflammation and cell death are prevalent.
The research team utilized 252 bacterial isolates from the human microbiome, sourced from the Australian Microbiome Culture Collection (AusMiCC). These isolates were grown in anaerobic chambers and treated with ten different compounds to assess their effects. The researchers characterized 134 inducible prophages from these isolates, expanding the knowledge of temperate phage–host interactions in human gut microbiology. Notably, only 18% of the computationally predicted prophages could be induced in pure cultures.
The findings indicated that most gut bacteriophages are dormant, with only a small fraction capable of activation under the tested conditions. However, exposure to human gut cells significantly increased the activation rate of these viruses. In a notable experiment, the team constructed a 78-member synthetic microbiome that, when co-cultured with human colonic cells (Caco2), resulted in the induction of 35% of phage species. This suggests that human biology plays a crucial role in shaping the viral landscape of the gut.
Among the activators identified, Stevia, a common plant-based sugar substitute, emerged as a key factor along with other compounds released by gut cells. “We’ve known that the gut is full of viruses, but until now, we didn’t have the tools and experimental approaches to study them in the lab,” explained Sofía Dahlman, a graduate student in Barr’s lab. “Our findings suggest that the human host isn’t just a passive environment; it’s actively influencing viral behavior.”
Utilizing CRISPR-based genetic engineering, the team identified mutations in viral genes that prevent activation. This insight could inform future therapeutic strategies aimed at manipulating the gut microbiome for health benefits. “Being able to grow these viruses allows us to understand their function and provides the opportunity to develop microbiome therapeutics for diseases from inflammatory bowel disease to cancers,” noted Forster, a researcher involved in the study.
This groundbreaking study not only enhances our understanding of the virome within the human gut but also opens avenues for developing targeted probiotics and therapies aimed at improving gut health. The implications of these findings could extend to a variety of health conditions, suggesting a complex interplay between the human microbiome and viral agents.