A recent study has unveiled a small protein that could revolutionize the identification and treatment of severe bone infections caused by the bacterium Staphylococcus aureus. Researchers at the University of Rochester Medical Center published their findings in the journal mBio on November 12, 2025, highlighting the potential of the protein, known as CCL20, in improving patient outcomes for those at risk of life-threatening infections.
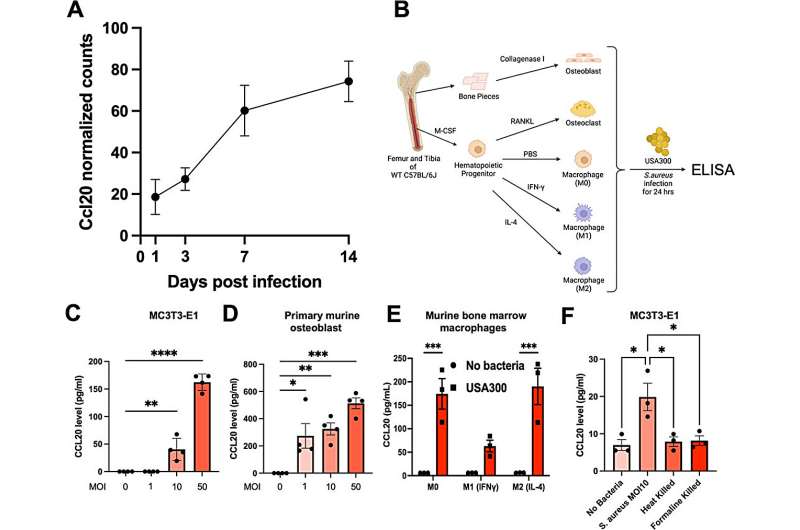
The research team focused on the role of CCL20 in bone infections, particularly osteomyelitis, which can lead to serious health complications, including septic shock. The study found that CCL20 levels increased progressively following infection in mice, suggesting its involvement in the immune response. Mice that lacked CCL20 experienced more severe infections and larger abscesses, indicating the protein’s critical role in fighting off infections.
In addition to understanding its role in infections, researchers discovered that CCL20 levels were significantly elevated in patients who developed bone infections after hip or knee replacement surgeries. In healthy individuals, the chemokine showed minimal presence, but in infected patients, levels surged fivefold, reaching an alarming 100 times the normal level in those who succumbed to sepsis. This indicates that CCL20 may serve as an important biomarker, providing a simple blood test to assess the severity of bone infections.
Dr. Gowrishankar Muthukrishnan, an assistant professor in Orthopedics and Microbiology & Immunology at the University of Rochester, emphasized the urgency of developing effective treatments for staph infections. “Treating a staph infection quickly offers patients the best chance at recovery and can prevent the risk of sepsis, which can cause death in a matter of hours,” he stated. He noted that despite advancements in medical technology, there has been no significant improvement in treatment or diagnostic methods for bone infections in over two decades.
The implications of this research are profound, especially considering that approximately 2 million total joint replacements occur annually in the United States. While the majority of these procedures are successful, the risk of osteomyelitis looms large as a post-operative complication. Patients can experience severe bone loss, require revision surgeries, or even face life-threatening conditions like sepsis.
The healthcare burden associated with bone infections is escalating. With an aging population and a growing number of joint replacements, projections indicate that by 2030, there could be up to 200,000 prosthetic joint infections annually in the U.S. alone, resulting in an estimated $3 billion in healthcare costs.
Dr. Himanshu Meghwani, the first author of the study and a staff scientist at the Center for Musculoskeletal Research, highlighted the potential of CCL20 not just as a diagnostic tool, but also as a therapeutic agent. The protein’s ability to recruit immune cells to the site of infection could enhance the body’s natural defenses. However, the research also revealed complexities, as some patients with high CCL20 levels still experienced severe infections and sepsis.
As the study progresses, researchers aim to deepen their understanding of CCL20’s mechanisms and its implications for both diagnosis and treatment. The promise of a simple blood test to monitor infection levels could prove invaluable for surgeons and patients alike, paving the way for improved surgical outcomes and potentially saving lives.