In a significant shift in women’s health care, doctors in Pennsylvania are leveraging mammograms, typically used for breast cancer screening, to identify early signs of heart disease. Health care providers across the region, including South Jersey and Delaware, are examining calcium buildup in the breast’s blood vessels, a condition known as breast arterial calcification (BAC). This development highlights a growing understanding of the connection between breast health and cardiovascular risks.
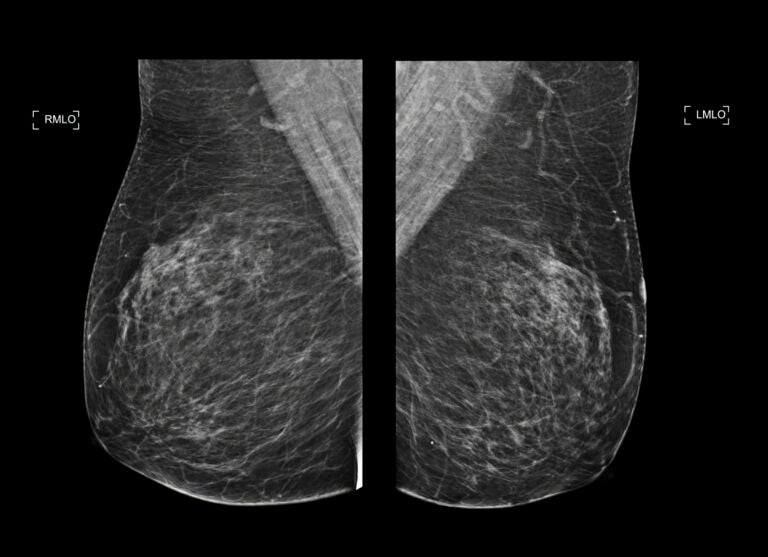
Traditionally, mammograms have been recommended for women starting at age 40 to screen for breast cancer. Now, physicians are recognizing that the imaging tests can also reveal critical information about heart health. The calcium deposits appear as fine bright white lines or clusters on X-ray images. Dr. Matthew Nudy, a noninvasive cardiologist and assistant professor at Penn State College of Medicine, notes that recent research has clarified the association between these deposits and cardiovascular disease.
According to Dr. Nudy, the presence of BAC indicates a higher risk of heart attack, stroke, or other cardiovascular complications as women age. He believes that informing patients about their BAC levels could lead to better heart health outcomes and a reduction in serious cardiac events. “If a patient knows that they have a BAC, they may be more in tune with what their blood pressure is, they may be more likely to get medications, they may be more aware of their health,” he stated.
Understanding the Significance of BAC
Calcium buildup is a well-known risk factor for cardiovascular disease, typically assessed through coronary artery calcium scans, a form of noninvasive CT imaging. Significant buildup prompts physicians to recommend lifestyle modifications or medications such as statins. Mammograms, while primarily focused on breast health, can also indicate the presence of BAC, which leads to stiffer blood vessels—another marker of heart disease.
Dr. Nudy emphasizes that many women over 40 undergo mammograms more frequently than coronary artery calcium scans. “It’s already being done for breast cancer screening across large numbers of patients in the population,” he explained, suggesting that this established practice could help bridge the gap in heart disease detection.
In August 2022, Jefferson Health hospitals in the Greater Philadelphia area began integrating BAC information into their mammogram screening reports. Patients receive educational materials prior to their screening, detailing what BAC is and the implications of the findings. Dr. Jason Shames, assistant professor of radiology at Thomas Jefferson University, described this approach as an educational opportunity that helps patients understand their health without adding unnecessary anxiety to an already stressful experience.
Moving Forward with Heart Health Awareness
Radiologists at Jefferson review all mammogram images for BAC and inform patients about their status in the report. This proactive communication allows healthcare providers to connect patients to specialists for further cardiovascular evaluation. Jefferson Health has also partnered with Solis Mammography to offer the Mammo+Heart program, which utilizes artificial intelligence to enhance the analysis of BAC in mammogram images. This service is available for patients willing to pay an additional fee for the more detailed assessment.
While the absence of BAC on a mammogram does not guarantee that a person is free from heart disease risk, it presents an important opportunity for women to identify potential early signs. Dr. Shames advocates for ongoing conversations between patients and their primary care teams regarding their health, particularly as they approach middle age.
Dr. Nudy aims to gather data on how BAC notifications influence patients’ health decisions. He is interested in whether knowledge of BAC leads to increased use of medications like statins, healthier lifestyle choices, and ultimately, a decrease in heart attacks and strokes over time.
The integration of mammograms as a tool for detecting heart health risks marks an important evolution in women’s health care, potentially empowering patients to take control of their cardiovascular health.






