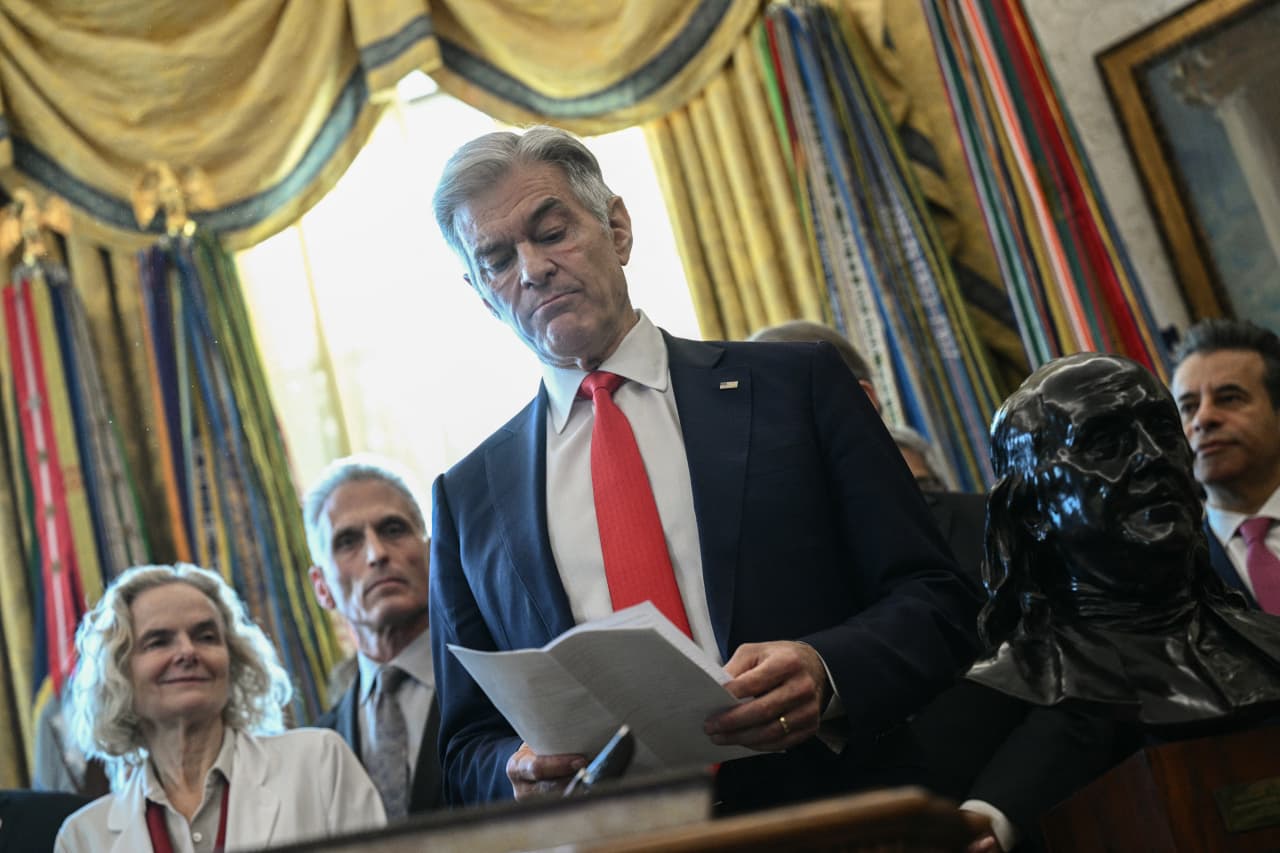
The landscape of treatment for non-small cell lung cancer (NSCLC) is evolving, as recent insights indicate that novel strategies could enhance responses in patients who do not benefit from standard immunotherapy. During the 26th Annual International Lung Cancer Congress, Dr. Hossein Borghaei, chief of the Division of Thoracic Medical Oncology at Fox Chase Cancer Center, presented findings suggesting that approaches such as JAK2 inhibitors, bispecific antibodies, and advanced cancer vaccines may offer new hope for these patients.
Dr. Borghaei emphasized the challenges faced by current treatments, noting that multiple phase 3 clinical trials have not successfully surpassed the efficacy of standard-of-care (SOC) options. “Based on small studies, we have a fairly consistent picture of the types of mechanisms of resistance that we can anticipate in patients who have disease progression with immunotherapy,” he explained. He identified that these mechanisms can be cancer cell dependent, immune related, or host related.
The presentation included data from the prospective phase 3 **Pragmatica-Lung (SWOG S2302)** study, which assessed the effectiveness of combining ramucirumab (Cyramza) with pembrolizumab (Keytruda) compared to SOC in patients with stage IV or recurrent NSCLC who had previously received immunotherapy. According to findings presented at the March 2025 ASCO Annual Meeting, the combination therapy did not yield a significant improvement in overall survival (OS) compared to SOC. The hazard ratio was calculated at 0.99 with a confidence interval of 95% (0.81-1.22) and a p-value of 0.46, indicating minimal difference between the two treatment arms.
“The OS in this study wasn’t that much better in the investigational arm vs SOC chemotherapy; perhaps this isn’t a good approach,” Dr. Borghaei stated, highlighting a need for alternatives.
Encouraging results have emerged from investigations into bispecific antibodies. The phase 3 **HARMONi-A study** demonstrated a marked increase in progression-free survival (PFS) for patients with nonsquamous NSCLC treated with the PD-1/VEGF bispecific antibody ivonescimab in conjunction with chemotherapy. The median PFS was reported at 7.1 months for the treatment group compared to 4.8 months for the placebo group, achieving a statistically significant result (p < 0.001). Dr. Borghaei acknowledged that while these findings are promising, they stem from a population with EGFR-positive disease, and further studies are required to validate these results across broader patient demographics. Additionally, he discussed a phase 2 study exploring the combination of JAK inhibition and anti-PD-1 therapy in treatment-naive metastatic NSCLC. Patients with PD-L1 levels of at least 50% receiving pembrolizumab together with the selective JAK1 inhibitor itacitinib exhibited a 12-week overall response rate of 62%. With a median follow-up of 27.6 months, the median PFS reached 23.8 months, showcasing a significant clinical benefit.
In the realm of cancer vaccines, the latest generation appears to offer more potential than previous iterations. A phase 1 trial investigating the use of an intratumoral adenovirus–IL-12 alongside atezolizumab (Tecentriq) revealed a disease control rate of 50% and a median PFS of 2 months among participants. Importantly, this combination showed no severe adverse effects, indicating a favorable safety profile.
Dr. Borghaei pointed to ongoing research with the therapeutic cancer vaccine OSE2101, which is currently undergoing evaluation against docetaxel in a phase 3 study targeting patients with metastatic NSCLC who exhibit secondary resistance to immunotherapy. The primary endpoint focuses on overall survival, with recruitment underway in North America and Europe.
“These are going to be important studies for us to pay attention to because they could offer a potential step forward,” he remarked, reinforcing the significance of this research.
Concluding his presentation, Dr. Borghaei reiterated the potential of bispecific antibodies to overcome resistance in NSCLC patients. “I believe something happens biologically when you engage multiple tumor antigens. Bispecifics could change the calculus,” he stated, suggesting that advancements might lead to more substantial improvements in patient outcomes compared to current SOC treatments.
As the field of lung cancer therapy continues to evolve, these innovative approaches may reshape treatment paradigms, providing new avenues for patients previously deemed resistant to existing immunotherapies.