The deadline for enrolling in a marketplace plan through the Affordable Care Act (ACA) for 2026 has passed, leaving millions of Americans facing the prospect of significant health care cost increases. Without an agreement on federal subsidies that help make ACA plans affordable, many individuals relying on these subsidies will see their health care expenses rise sharply in the coming year. This situation follows a last-minute effort in the House to extend ACA subsidies, which ultimately failed as Congress adjourned for the year on December 19, 2025.
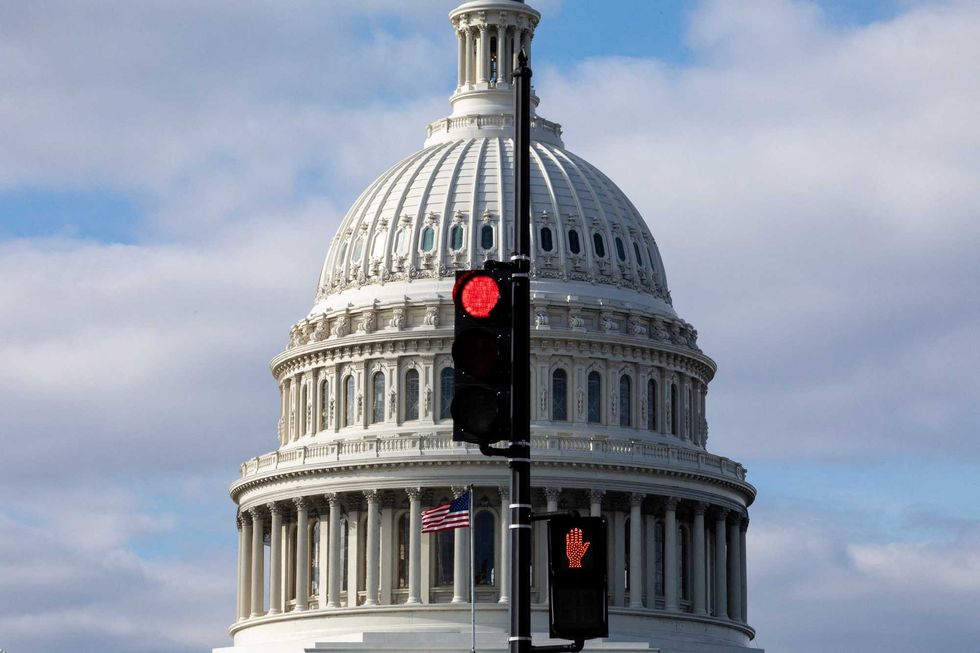
The ACA, enacted in 2010, represents a crucial chapter in the ongoing debate about whether health care should be a governmental responsibility or an individual one. Disagreements surrounding this issue have led to political divisiveness, including a recent government shutdown that lasted 43 days, beginning on October 1, 2025. As a gerontologist studying the U.S. health care system, I recognize that a sustainable health care policy will remain elusive until lawmakers address the central question of who bears the cost of health care.
The Roots of the ACA
Prior to the ACA’s implementation, approximately 49 million Americans, or 15 percent of the population, were uninsured—a number that had been increasing since the 2008 recession. Most individuals aged 18 to 64 obtain health insurance through their employers; thus, job losses during the recession led to corresponding losses in health coverage. Advocates for government involvement argued that this growing number of uninsured citizens indicated a crisis requiring intervention, while opponents viewed the ACA as a misstep for government overreach.
The ACA aimed to reduce the number of uninsured Americans by about 30 million, ultimately achieving a decrease to around 26 million, or 8 percent, of the population. This progress fluctuates based on economic conditions and policy changes. The legislation introduced measures to expand health insurance coverage, including allowing young adults to remain on their parents’ insurance until age 26 and mandating that all individuals obtain insurance.
One of the most significant components of the ACA was the expansion of the Medicaid program to include low-income workers earning below 138 percent of the federal poverty line. Initially mandated for all states, the U.S. Supreme Court ruled that it was up to individual states to decide on implementation. As of December 2025, 40 states and the District of Columbia have adopted Medicaid expansion, providing coverage for approximately 20 million Americans.
Implications of Expiring Subsidies
The ACA also included subsidies aimed at assisting low- and middle-income individuals in purchasing health insurance through the ACA marketplace. In 2021, the Biden administration expanded these subsidies in response to the COVID-19 pandemic, eliminating premiums for the lowest-income individuals and allowing those earning above the previous threshold to qualify. These enhanced subsidies are set to expire at the end of 2025, potentially leading to substantial cost increases for many consumers.
For instance, an individual earning $45,000 annually could see their monthly insurance premium rise by 74 percent, from approximately $360 to around $513. This increase is compounded by projected insurance price hikes of about 18 percent in 2026. Together, these factors could result in many ACA marketplace users experiencing cost increases of over 100 percent.
Advocates for extending the COVID-19-era subsidies warn that failing to do so could push 6 million to 7 million people out of the ACA marketplace, with about 5 million likely to become uninsured by 2026. Additionally, recent policies included in a tax and spending package signed by former President Donald Trump in July 2025 are expected to exacerbate the issue, with the Congressional Budget Office projecting that Medicaid cuts alone could result in more than 7 million people becoming uninsured.
Critics of the enhanced subsidies argue that they have significantly increased federal health care expenditures, with the number of subsidy recipients doubling between 2021 and 2024. In 2025, nearly 22 million Americans receiving marketplace plans benefited from federal subsidies, representing a 137 percent increase from 9.2 million in 2020. Opponents contend that these subsidies disproportionately assist higher-income individuals and question whether temporary measures should lead to enduring changes in the health care system.
Moreover, there are concerns that employers are using the ACA to diminish their responsibility to provide health coverage. Data shows a decline in health care offerings from employers with 25 to 49 employees—from 92 percent in 2010 to 64 percent in 2025—indicating that many companies may rely on the ACA to cover their workers instead.
The U.S. health care system is the most expensive in the world. Experts warn that the anticipated rise in uninsured individuals could lead to increased costs over time, as fewer people receive preventive care and delay necessary medical interventions, resulting in more complex health issues.
While national policies significantly influence health insurance coverage, state-level decisions also play a critical role. In 2023, approximately 8 percent of individuals under age 65 were uninsured nationally, but this rate varied significantly by state—from 3 percent in Massachusetts to 18.6 percent in Texas. States governed by Republican leaders generally have higher percentages of uninsured residents compared to those led by Democrats, reflecting the broader political divide over health care responsibilities.
The ongoing debate over who should bear the cost of health care continues to present challenges. Advocates for increased government support argue for expanded coverage funded by taxes, while those favoring individual responsibility propose market-driven solutions. Without a resolution to this enduring question, the United States is likely to face continued contention regarding health care policy for years to come.







