Significant advancements in gene editing technology, particularly the CRISPR-Cas9 system, may pave the way for novel treatments of genetic disorders. Recent findings from researchers at the Gladstone Institutes, the Innovative Genomics Institute, and UC Berkeley reveal that neurons and other nondividing cells exhibit distinct responses to gene editing compared to dividing cells. This discovery could reshape how therapies targeting brain-related genetic conditions are designed.
In a study published in Nature Communications on November 18, 2025, researchers led by Bruce Conklin, MD, a Senior Investigator at Gladstone, identified key differences in the DNA repair mechanisms between these cell types. “If we want to ensure genome edits result in the right outcomes, we need to understand and control how the cell’s DNA is repaired after we cut it,” Conklin stated.
Exploring the Differences in DNA Repair
CRISPR-Cas9 operates by using a protein called Cas9, which acts as molecular scissors to cut DNA at specific sites. The study found that neurons reacted differently to CRISPR interventions than the dividing cells typically used in previous research. Gokul Ramadoss, a Ph.D. candidate and lead author of the study, explained, “Most people studying CRISPR have focused on dividing cells, but it turns out the rules of genome editing are different in nondividing cells like neurons.”
The study emphasized that while the same DNA was targeted, the outcomes varied significantly. In neurons, the effects of Cas9 persisted longer, with editing continuing for approximately one month, compared to just a few days in dividing induced pluripotent stem (iPS) cells. This prolonged presence of Cas9 in neurons raises new safety considerations. “If Cas9 hangs around longer, it has more chances to do its job and make on-target edits, which we want,” Conklin noted. “But it also has more chances to make off-target edits, which we don’t want.”
Innovative Strategies for Gene Editing
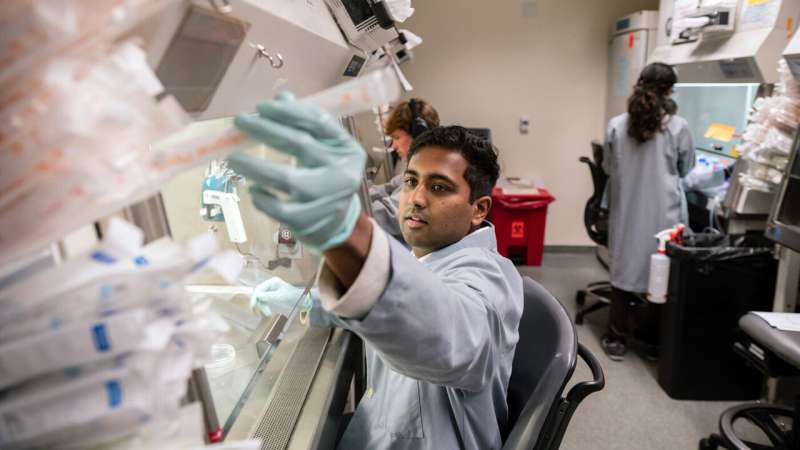
To study these differences, the researchers successfully delivered controlled amounts of CRISPR-Cas9 molecules into neurons. This was accomplished in collaboration with Jennifer Doudna, Ph.D., a Nobel Prize-winning scientist recognized for her role in developing CRISPR technology. Doudna’s lab created nanoparticles known as “enveloped delivery vehicles,” which can safely transport gene-editing molecules into various cell types.
Through this collaborative effort, the team utilized iPS cells, which can be transformed into neurons, allowing a direct comparison between dividing and nondividing cells sharing the same genetic material. The results demonstrated that the DNA repair outcomes in neurons were limited to a narrower range of changes, leading to potentially more predictable editing results.
Conklin likened the editing process to repairing a masterpiece: “Imagine if someone slashed the Mona Lisa with a razor. Would you rather have many different people trying to put it back together all at once, or one dedicated expert who repairs it the same way every time?”
The findings revealed that edited neurons activated certain DNA repair genes previously thought to be inactive in nondividing cells. This insight could lead to new methods for directing gene editing towards more advantageous outcomes, potentially extending to other critical nondividing cells, such as heart muscle cells.
As the research evolves, the team is focused on developing strategies to manage these repair pathways effectively. Collaborating with Niren Murthy, Ph.D., a professor of bioengineering at UC Berkeley, the researchers designed lipid nanoparticles that can co-deliver gene editing tools alongside molecules that inhibit specific repair genes in neurons.
Ramadoss described this innovation as akin to performing surgery on the genome: “Before, we could make an incision but we couldn’t control how the DNA gets stitched up afterward. With this work, we’re starting to develop the repair tools required to ensure the right editing outcome.”
The implications of this research extend beyond neurons, providing a framework that could be adapted for various gene-editing proteins, other cell types, and multiple diseases. “Our ultimate goal is to precisely control the gene editing process to deliver life-changing therapies,” Conklin asserted. “And now, we have important new tools to make sure we get this right.”







